Virus Mimicking Antibodies May Explain Long Haul COVID-19, Rare Vaccine Side Effects
0 View
Share this Video
- Publish Date:
- 27 November, 2021
- Category:
- Covid
- Video License
- Standard License
- Imported From:
- Youtube
Tags
With approximately 256 million cases and more than 5 million deaths worldwide, the COVID-19 pandemic has challenged scientists and people in the medical field. Researchers are working to find effective vaccines and therapies, as well as understanding the long-term effects of the infection.
While the vaccines have been critical in fighting the pandemic, researchers are still learning how and how well they work. This is especially true for the emergence of new viral variants and the rare side effects of the vaccine, such as allergic reactions, inflammation of the heart (myocarditis) and blood clotting (thrombosis).
Critical questions also remain about the infection itself. About one in four COVID-19 patients have persistent symptoms even after recovering from the virus. These symptoms, known as “prolonged COVID,” and the side effects of the off-target vaccines, are thought to be caused by a patient’s immune response.
In an article published Nov. 24, 2021 in The New England Journal of Medicine, UC Davis Vice Chair of Research and Distinguished Professor of Dermatology and Internal Medicine William Murphy and Professor of Medicine at Harvard Medical School Dan Longo present a possible explanation for the various immune responses to the virus and vaccines.
Antibodies that mimic the virus
Based on classical immunological concepts, Murphy and Longo suggest that Nobel laureate Niels Jerne’s network hypothesis could provide insights.
Jerne’s hypothesis describes a means for the immune system to regulate antibodies. It describes a cascade in which the immune system initially launches protective antibody responses against an antigen (such as a virus). These same protective antibodies can later trigger a new antibody response against themselves, causing them to disappear over time.
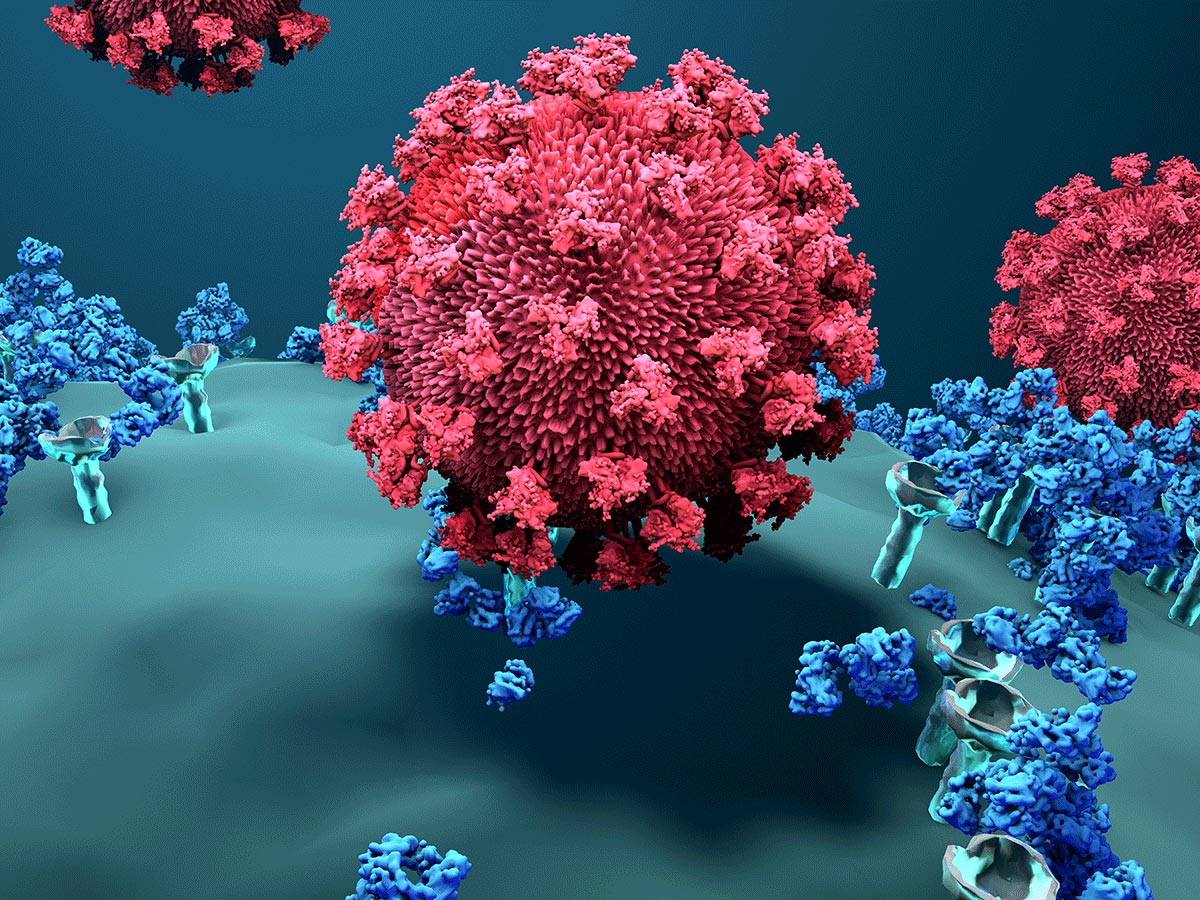
The spike protein mediates the entry of the coronavirus into host cells.
These secondary antibodies, termed anti-idiotype antibodies, can bind to and deplete the initial protective antibody responses. They have the potential to mirror or behave in the original antigen itself. This can lead to adverse effects.
Coronavirus and the immune system
When SARS-CoV-2, the virus that causes COVID-19, enters the body, the spike protein binds to the ACE2 receptor and enters the cell. The immune system responds by producing protective antibodies that bind to the invading virus, blocking or neutralizing its effects.
As a form of down-regulation, these protective antibodies can also cause immune reactions with anti-idiotype antibodies. Over time, these anti-idiotype responses can remove the initial protective antibodies and potentially result in limited efficacy of antibody-based therapies.
“A fascinating aspect of the newly formed anti-idiotype antibodies is that some of their structures may mirror the original antigen and behave like that by binding to the same receptors that the viral antigen binds. This binding could potentially lead to to undesired actions and pathology, especially in the long term,” Murphy said.
The authors suggest that the anti-idiotype antibodies may target the same ACE2 receptors. By blocking or activating these receptors, they can affect several normal ACE2 functions.
“Given the critical functions and wide distribution of ACE2 receptors on numerous cell types, it would be important to determine whether these regulatory immune responses could be responsible for some of the off-target or long-lasting effects being reported,” Murphy noted. . “These responses may also explain why such long-term effects can occur long after the viral infection is over.”
As for COVID-19 vaccines, the primary antigen used is the SARS-CoV-2 spike protein. According to Murphy and Longo, current studies of antibody responses to these vaccines focus on the initial protective responses and virus neutralizing efficacy, rather than other long-term aspects.
“With the incredible impact of the pandemic and our reliance on vaccines as our primary weapon, there is a tremendous need for more basic science research to understand the complex immunological pathways at play. This need follows what is needed to maintain the protective responses, as well as the potential unwanted side effects of both the infection and the different SARS-CoV-2 vaccine types, especially as boosting is now being applied,” Murphy said. good news is that these are testable questions that can be answered in part in the lab and have in fact been used with other viral models.”
Reference: “A possible role for anti-idiotype antibodies in SARS-CoV-2 infection and vaccination” by William J. Murphy, Ph.D. and Dan L. Longo, MD, Nov. 24, 2021, New England Journal of Medicine.
DOI: 10.1056/NEJMcibr2113694










