Tiny Hairlike Structures Could Help Treat Lung Illnesses Like COVID-19
0 View
Share this Video
- Publish Date:
- 24 July, 2021
- Category:
- Covid
- Video License
- Standard License
- Imported From:
- Youtube
Tags
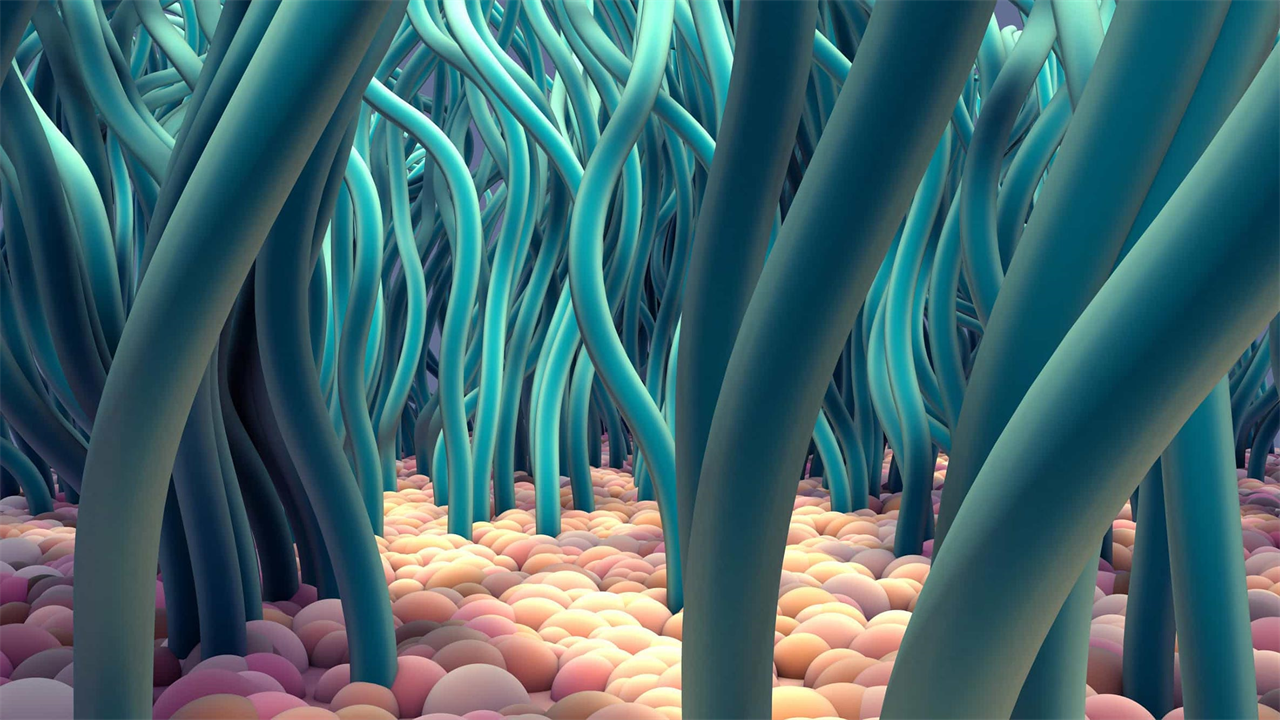
3D image of ciliated cells.
With an NIH award of $2.3 million, USC researchers will study how the behavior and structure of cilia influence their function, a key in improving diagnostics and treatments for lung diseases such as COVID-19.
Cilia, microscopic hair-like structures found along the bronchi (air passages through the lungs), are the first line of defense against environmental pollutants, viruses and bacteria. But we know little about how they’re arranged, how they move, or even how they’re oriented — all factors that likely influence how well they defend and protect our airways.
With support from the National Institutes of Health, researchers at USC’s Viterbi School of Engineering and USC’s Keck School of Medicine are working to bridge mathematical models of cilia behavior to biological and pathological (disease-causing) consequences. In other words, they hope to better understand how changing a variable in how cilia beat or how it’s distributed can affect a person’s health.
The study leaders are Eva Kanso, USC Viterbi professor of aerospace and mechanical engineering, and Amy Ryan, assistant professor of medicine at Keck.
Kanso, Zohrab A. Kaprielian Fellow in Engineering, said: “We want to understand first what the normal variations are for healthy lungs and then understand the pathological variations. If we can link these observations to the underlying pathology, we can better understand how the structure of cilia – distribution, coordination, polarity, density – can affect actual function – how they move mucus, how well they disappear in a particular direction.”
The team looks at cilia from three perspectives, Kanso said. “First, we’re looking at real human lungs, which is very current right now given COVID-19,” she said. “There are so many questions we don’t know the answers to, such as the distribution of cilia from the upper respiratory tract to when they begin to branch into smaller branches. The distribution varies depending on where you are in the lungs.
Mathematical modeling of cilia to answer important questions
In Kanso’s lab, this exploration is done by means of mathematical models. “We have models of individual cilia and we combine them together to look at the coordination of a series of cilia. We look at function and transport flow, manipulating all kinds of parameters,” she said.
Cilia spontaneously coordinate to create a wave pattern, Kanso said, which is important for fluid transport. “There’s a definite direction the wave is moving in that sweeps away everything (bacteria, etc.) in the direction of that moving wave.”
In the mathematical model, Kanso said, you can change the distance between cilia, individual beats, polarity, etc. and see how it shifts the coordination that arises and ultimately the corresponding function of the cilia and its transport flow. Parameters that negatively affect the wave pattern can provide clues about how diseased lungs look and function, she said.
Impact on human health
From a biological perspective, this research could provide important new insights into inherited and acquired respiratory diseases characterized by cilia dysfunction, Ryan said.
“In addition to significantly increasing our understanding of the impact of disease on airway functional properties, the development of mathematical models could potentially be applied in the diagnosis of ciliopathy to predict disease progression.” Current diagnostic techniques require very specific scientific expertise, Ryan said, which makes them challenging.
“Looking ahead, our long-term goal is to combine laboratory models with computer models to create a medical tool that can help evaluate therapies targeting lung diseases characterized by poor mucociliary clearance – or malfunctioning of the self-purification methodology in the airways,” Ryan said.
The NIH award is over $2.3 million for four years.










