Potential New COVID-19 Treatment: A Tapeworm Drug
0 View
Share this Video
- Publish Date:
- 27 June, 2021
- Category:
- Covid
- Video License
- Standard License
- Imported From:
- Youtube
Tags
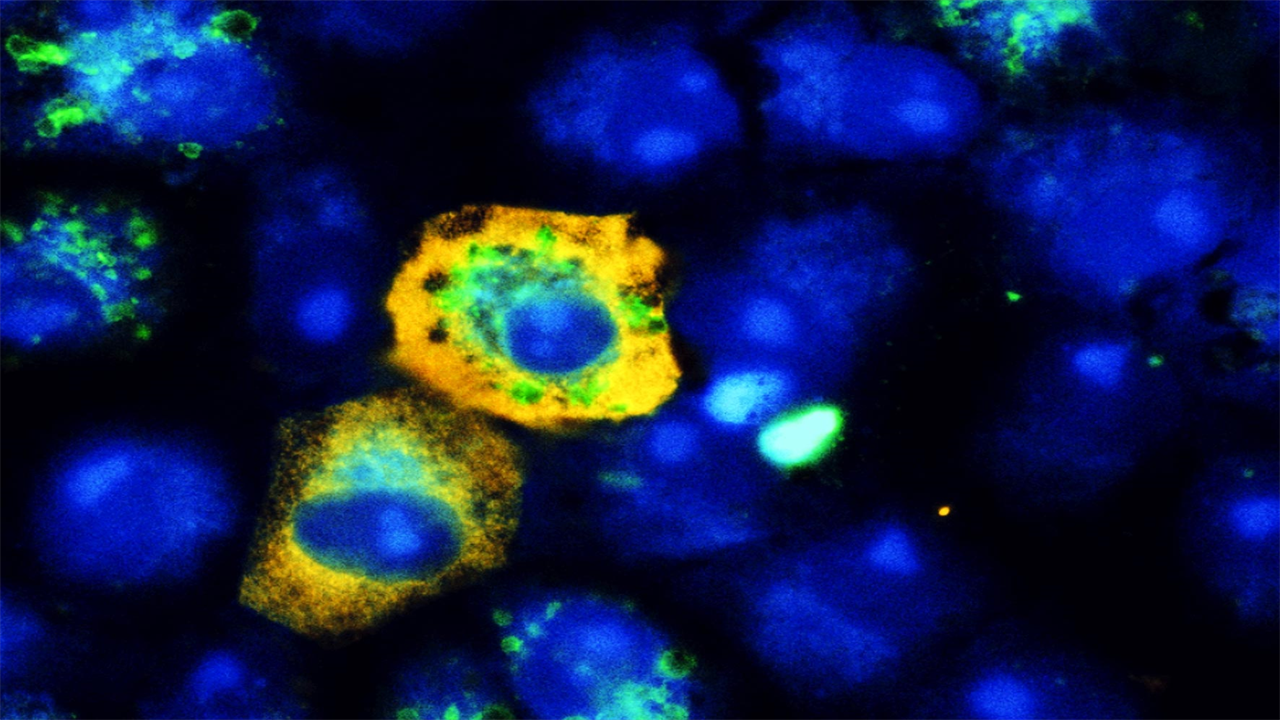
When SARS-CoV-2 (yellow) infects monkey kidney cells, it reduces the cellular recycling mechanism, meaning there are fewer autophagy signals (green) than in uninfected cells. Blue staining shows nuclei. Credit: © University Hospital Bonn | Daniel Heinz
Charité conducts clinical trial to test possible new treatment against SARS-CoV-2.
Researchers from the German Center for Infection Research (DZIF) of Charité – Universitätsmedizin Berlin and the University of Bonn have examined the way SARS-CoV-2 reprograms host cell metabolism to achieve an overall benefit. According to their report in Nature Communications, the researchers were able to identify four substances that inhibit the replication of SARS-CoV-2 in the host cell: spermine and spermidine, substances that occur naturally in the body; MK-2206, an experimental cancer drug; and niclosamide, a drug against tapeworms. Charité is currently conducting a trial to determine whether niclosamide is also effective against COVID-19 in humans.
Viral replication depends on the host cell’s machinery and the use of the host’s molecular building blocks. To avoid detection by the immune system, viruses must also ensure that they can evade cellular surveillance systems. To do this, they manipulate different processes in the infected host cell – and each virus follows a different strategy. This is why a team of researchers led by PD Dr. Marcel Müller of Charité’s Institute of Virology and Dr. Nils Gassen of the Psychiatry and Psychotherapy Clinic and Outpatient Clinic at University Hospital Bonn (UKB) have investigated the way SARS-CoV -2 reprograms host cells for its own benefit.
Their main finding was this: The novel coronavirus slows down the cell’s own recycling mechanism, a process known as autophagy. The goal of this ‘auto-digestion’ mechanism is to allow the cell to dispose of damaged cell materials and waste products and recycle useful molecular building blocks for incorporation into new cell structures.
“In our study, we were able to show that SARS-CoV-2 not only uses the building blocks of the cell for its own benefit, but also tricks the cell by simulating a nutrient-rich state, slowing down cellular recycling,” first explains. author Dr. Gassen. As part of this work, the researchers performed a detailed analysis of SARS-CoV-2 infected cells and the lung tissue of COVID-19 patients, studying cellular metabolism and molecular signal processing.
“Probably SARS-CoV-2 uses this to prevent disassembly by the cell. After all, viruses are also subject to autophagic elimination,” adds the study’s latest author, DZIF researcher PD Dr. Muller. He adds: “The same reprogramming strategy is also used by the MERS coronavirus, whose autophagy inhibitory activity we were able to demonstrate more than a year ago. However, there are other coronaviruses that, quite in contrast, induce autophagy. They mainly infect animals.”
When the results of the study suggested that the recycling mechanism could be a potential target for COVID-19 therapy, the researchers tested whether substances that induce cellular recycling also reduce SARS-CoV-2 replication in infected cells. Interestingly, the researchers found four substances that proved effective — all of which are already in use in humans. These include the polyamine spermidine, an autophagy-enhancing metabolite produced in all human cells and by bacteria in the human gut. It occurs naturally in foods such as wheat germ, soy, mushrooms and mature cheese and is available over the counter as a dietary supplement.
When the researchers added spermidine to SARS-CoV-2 infected cells, it resulted in an 85 percent reduction in the number of virus particles produced. Similar results were produced by spermine, another polyamine that occurs naturally in the body. This derivative of spermidine was found to reduce viral replication by more than 90 percent in human lung cells and in a human gut model containing clusters of cells known as “organoids.”
“The obvious effects of spermidine and spermine in particular are certainly encouraging. For starters, substances that occur naturally in the body are less likely to cause side effects,” says PD Dr. Muller. “That said, we were working with pure forms of these substances that are not suitable for medical use. Spermidine, in particular, must be used in relatively high concentrations to achieve a noticeable effect in cell culture.
“Therefore, many questions remain to be answered before we can consider polyamines as a potential treatment against COVID-19: When used in the body, will it be possible to achieve blood levels high enough to inhibit viral replication in the airways? And if so: is administration before or during the infection advisable? Are there any side effects? Nevertheless, our findings from cell culture are a good starting point for research with animal models. Self-medication is not recommended, one reason is that viruses also use polyamines to stimulate replication; the correct dosage is therefore crucial. The same goes for fasting, which can stimulate the body’s autophagy process. Since the body needs energy to mount an immune response, it remains unclear whether fasting is advisable in SARS-CoV-2 infected patients.”
The third substance that proved effective against SARS-CoV-2 was the ‘AKT inhibitor’ MK-2206. The substance is currently in the clinical trial phase and is being tested for its tolerability and efficacy against a range of different cancers. In the current study, MK-2206 reduced the production of infectious SARS-CoV-2 virus by approximately 90%. It did this at plasma concentrations already achieved in a previous study. “Based on our data, I would consider MK-2206 an interesting treatment candidate against COVID-19 that, after careful risk-benefit analysis, would warrant further study in clinical trials,” explains PD Dr. Muller out.
The most pronounced antiviral activity was associated with niclosamide, which the researchers had shown in a previous study to be effective against the MERS coronavirus. The tapeworm drug was found to reduce the production of infectious SARS-CoV-2 particles by more than 99 percent.
“Niclosamide showed the strongest effect in our cell culture-based experiments. In addition, it has long been approved for use against tapeworm infections in humans and is well tolerated in potentially relevant doses,” says PD Dr. Muller. He adds: “Of the four new candidate compounds, we consider this to be the most promising. That is why we are now conducting a clinical trial at Charité to test whether niclosamide may also have a positive effect on people with COVID-19. I am delighted with this development. It shows how quickly findings from basic research can reach patients when research and clinical practice are closely linked and work together in an efficient way.”
The Phase II clinical trial – titled ‘NICCAM’ – is led by Prof. dr. dr. Martin Witzenrath, deputy head of Charité’s Infectious Diseases and Respiratory Medicine Department. The study will test the safety, tolerability and efficacy of niclosamide in combination with camostat (another licensed drug) in patients recently (within the past few days) diagnosed with COVID-19. The study is currently recruiting and searching for participants. Potential participants wishing to learn more about the study can contact the Charité Research Organisation’s team on +49 30 450 539 210 or by emailing patients(at)charite-research.org.
Reference: “SARS-CoV-2-mediated dysregulation of metabolism and autophagy reveals host-targeting antivirals” by Nils C. Gassen, Jan Papies, Thomas Bajaj, Jackson Emanuel, Frederik Dethloff, Robert Lorenz Chua, Jakob Trimpert, Nicolas Heinemann, Christine Niemeyer, Friderike Weege, Katja Hönzke, Tom Aschman, Daniel E. Heinz, Katja Weckmann, Tim Ebert, Andreas Zellner, Martina Lennarz, Emanuel Wyler, Simon Schroeder, Anja Richter, Daniela Niemeyer, Karen Hoffmann, Thomas F. Meyer, Frank L Heppner, Victor M. Corman, Markus Landthaler, Andreas C. Hocke, Markus Morkel, Nikolaus Osterrieder, Christian Conrad, Roland Eils, Helena Radbruch, Patrick Giavalsco, Christian Drosten and Marcel A. Müller, June 21, 2021, Nature Communications.
DOI: 10.1038/s41467-021-24007-w










