NIH Scientists Identify Mechanism That May Boost Infectivity of COVID Variants
0 View
Share this Video
- Publish Date:
- 10 November, 2021
- Category:
- Covid
- Video License
- Standard License
- Imported From:
- Youtube
Tags
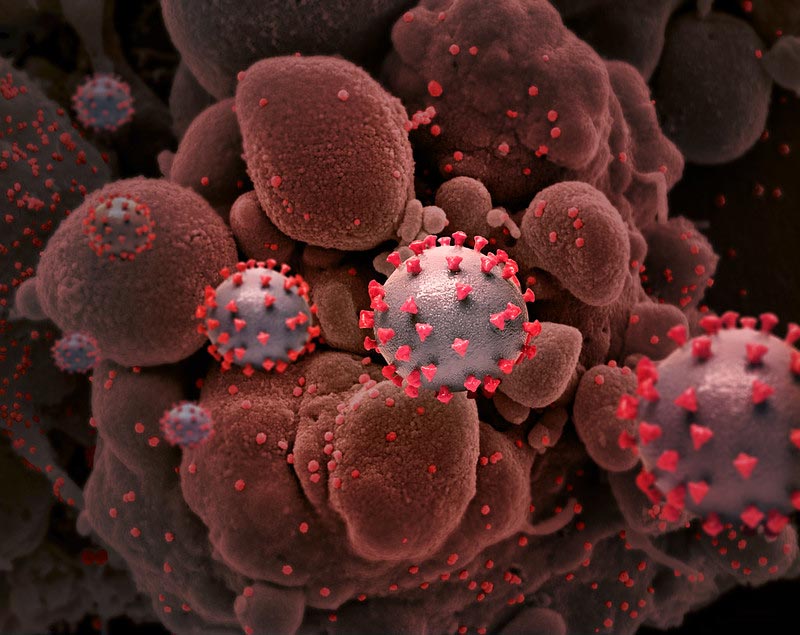
Creative representation of SARS-COV-2 virus particles with spike proteins on their surface. Image not to scale. Credit: National Institute of Allergy and Infectious Diseases, NIH
Enzyme process changes the function of spike protein.
Scientists at the National Institutes of Health have discovered that a process in cells can limit the infectivity of SARS-CoV-2, and that mutations in the alpha and delta variants negate this effect, potentially allowing the virus to spread. The findings are published online in the Proceedings of the National Academy of Sciences. The study was led by Kelly Ten Hagen, Ph.D., a senior researcher at NIH’s National Institute of Dental and Craniofacial Research (NIDCR).
Since the coronavirus pandemic began in early 2020, several more contagious variants of SARS-CoV-2, the virus that causes COVID-19, have emerged. The original, or wild-type, virus was followed by the alpha variant, which became widespread in the United States in early 2021, and then the delta variant, the most common strain circulating today. The variants have been given mutations that allow them to infect humans and spread more easily. Many of the mutations affect the spike protein, which the virus uses to get into cells. Scientists have been trying to understand how these changes alter the function of the virus.
“During the pandemic, NIDCR researchers have applied their expertise in oral health sciences to answer important questions about COVID-19,” said NIDCR Director Rena D’Souza, DDS, Ph.D. “This study provides new insights into the greater infectivity of the alpha and delta variants and provides a framework for the development of future therapies.”
The outer surface of SARS-CoV-2 is decorated with spike proteins, which the virus uses to attach to and invade cells. Before this can happen, however, the spike protein must be activated through a series of cuts or cleavage through host proteins, starting with the furin enzyme. In the alpha and delta variants, mutations in the spike protein appear to enhance furin cleavage, which is thought to make the virus more effective at entering cells.
Studies have shown that protein splicing can be reduced in some cases by adding bulky sugar molecules — a process performed by enzymes called GALNTs — next to the cleavage site. Ten Hagen’s team wondered whether this happens with the SARS-CoV-2 spike protein, and if so, whether it changes the function of the protein.
To find out, the scientists studied the effects of GALNT activity on spike protein in fruit fly and mammalian cells. The experiments showed that one enzyme, GALNT1, adds sugars to wild-type spike protein, and this activity reduces furin cleavage. In contrast, mutations in the spike protein, such as those in the alpha and delta variants, decrease GALNT1 activity and increase furin cleavage. This suggested that GALNT1 activity can partially suppress furin splicing in wild-type virus, and that the alpha and delta mutations overcome this effect, leaving furin splicing uncontrolled.
Further experiments supported this idea. The researchers expressed either wild-type or mutated spike in cells grown in a dish. They observed the tendency of the cells to fuse with their neighbors, a behavior that may facilitate the spread of the virus during infection. The scientists found that cells expressing mutated spike protein fused with neighbors more often than cells with the wild-type spike. Wild-type spike cells also fused less frequently in the presence of GALNT1, suggesting that the activity may limit spike protein function.
“Our findings indicate that the alpha and delta mutations negate the dampening effect of GALNT1 activity, which could improve the virus’s ability to penetrate cells,” Ten Hagen said.
To see if this process can also occur in humans, the team analyzed RNA expression in cells from healthy volunteers. The researchers found broad expression of GALNT1 in lower and upper respiratory tract cells susceptible to SARS-CoV-2 infection, indicating that the enzyme could influence infection in humans. The scientists theorized that individual differences in GALNT1 expression could influence virus spread.
“This study suggests that GALNT1 activity may modulate viral infectivity and provides insight into how mutations in the alpha and delta variants may affect this,” Ten Hagen said. The knowledge could contribute to future efforts to develop new interventions.
Reference: “Furin cleavage of the SARS-CoV-2 peak is modulated by O-glycosylation” by Liping Zhang, Matthew Mann, Zulfeqhar A. Syed, Hayley M. Reynolds, E. Tian, Nadine L. Samara, Darryl C Zeldin, Lawrence A. Tabak and Kelly G. Ten Hagen, Nov. 3, 2021, Proceedings of the National Academy of Sciences.
DOI: 10.1073/pnas.2109905118
This research was supported by the NIDCR Division of Intramural Research. Support also came from the National Institute of Environmental Health Sciences intramural program.










