“Nanodecoys” – Made From Human Lung Spheroid Cells – Bind and Neutralize SARS-CoV-2 (COVID-19) Virus
0 View
Share this Video
- Publish Date:
- 24 June, 2021
- Category:
- Covid
- Video License
- Standard License
- Imported From:
- Youtube
Tags
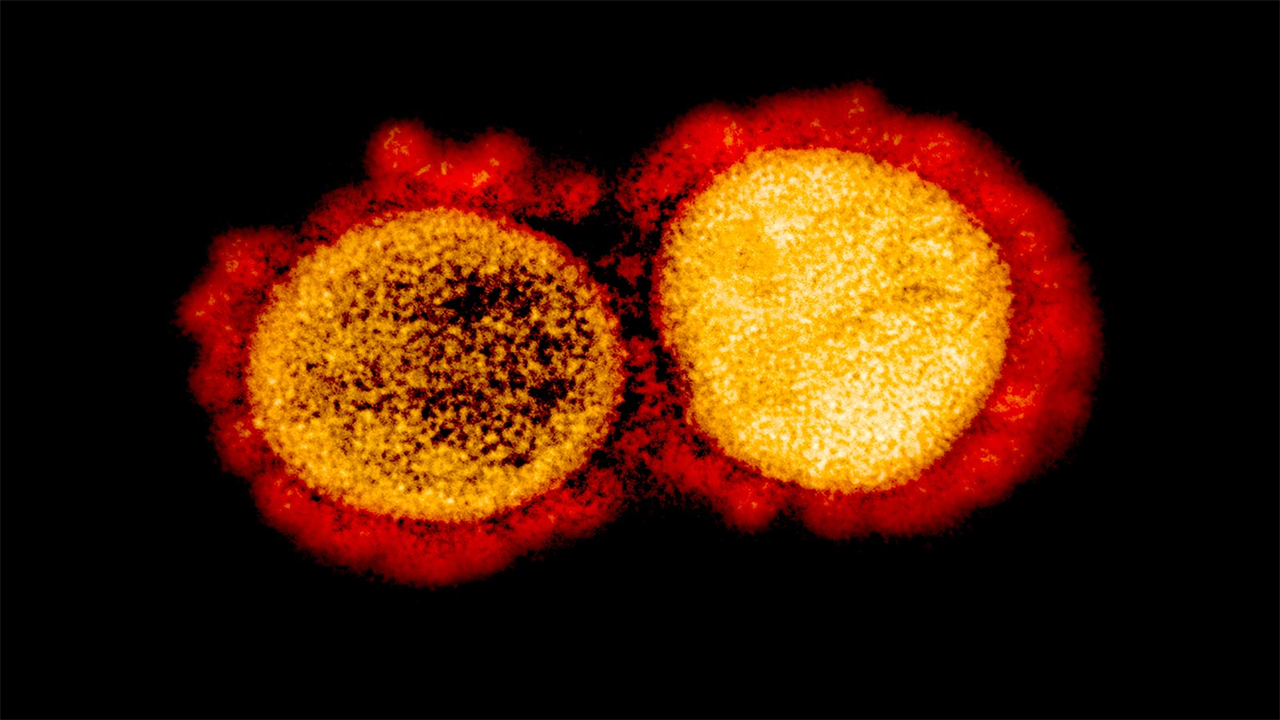
Transmission electron micrograph of SARS-CoV-2 virus particles isolated from a patient. Image captured and enhanced in color at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
Nanodecoys made from human spheroid lung cells (LSCs) can bind to and neutralize SARS-CoV-2, promote viral clearance and reduce lung damage in a macaque model of COVID-19. By mimicking the receptor the virus binds to rather than targeting the virus itself, nanodecoy therapy could remain effective against emerging variants of the virus.
SARS-CoV-2 enters a cell when the spike protein binds to the angiotensin-converting enzyme 2 (ACE2) receptor on the cell surface. LSCs – a natural mixture of lung epithelial stem cells and mesenchymal cells – also express ACE2, making them a perfect tool to trick the virus.
“If you think of the spike protein as a key and the cell’s ACE2 receptor as a lock, what we’re doing with the nanodecoys is showering the virus with fake locks so it can’t get to those who let it enter the lung cells find,” says Ke Cheng, corresponding author of the study. “The fake locks bind and trap the virus, preventing it from infecting cells and multiplying, and the body’s immune system takes care of the rest.”
“Nanodecoys” made from human spheroid lung cells (LSCs) can bind to and neutralize SARS-CoV-2, promoting viral clearance and reducing lung damage in a macaque model. Credit: Ke Cheng, NC State University
Cheng is the Randall B. Terry Jr. Distinguished Professor of Regenerative Medicine at North Carolina State University and a professor in the NC State/UNC-Chapel Hill Joint Department of Biomedical Engineering.
Cheng and colleagues at NC State and UNC-CH converted individual LSCs into nanovesicles, or small cell membrane bubbles with ACE2 receptors and other lung cell-specific proteins on the surface.
They confirmed that the spike protein bound to the ACE2 receptors on the decoys in vitro, and then used a manufactured SARS-Co-V-2 mimic virus for in vivo testing in a mouse model. The decoys were delivered via inhalation therapy. In mice, the nanodecoys remained in the lungs for 72 hours after a single dose and accelerated clearance of the mimic virus.
Finally, a contract research organization conducted a pilot study in a macaque model and found that inhalation therapy with the nanodecoys accelerated viral clearance and reduced inflammation and fibrosis in the lungs. While no toxicity was noted in the mouse or macaque study, further research will be needed to translate this therapy for human testing and determine exactly how the nano-decoys are eliminated by the body.
Nanodecoys bind with the SARS-CoV-2 virus. Credit: North Carolina State University
“These nanodecoys are essentially ‘ghosts’ of cells, and one LSC can generate about 11,000 of them,” Cheng says. “Deploying millions of these decoys exponentially increases the surface area of fake binding sites for trapping the virus, and their small size actually turns them into small bite-sized snacks for macrophages, so they are removed very efficiently.”
The researchers point to three other advantages of the LSC nanodecoys. First, they can be delivered non-invasively to the lungs via inhalation therapy. Second, since the nanodecoys are acellular – nothing lives in them – they can be stored easily and remain stable for longer, making them readily available. Finally, LSCs are already being used in other clinical trials, so they are more likely to be used in the near future.
“By focusing on the body’s defenses rather than a virus that continues to mutate, we have the potential to create a therapy that will be helpful in the long run,” Cheng says. “As long as the virus has to enter the lung cell, we can continue to cheat it.”
Reference: “Cell-mimicking nanodecoys neutralize SARS-CoV-2 and reduce lung damage in a non-human primate model of COVID-19” by Zhenhua Li, Zhenzhen Wang, Phuong-Uyen C. Dinh, Dashuai Zhu, Kristen D. Popowski, Halle Lutz, Shiqi Hu, Mark G. Lewis, Anthony Cook, Hanne Andersen, Jack Greenhouse, Laurent Pessaint, Leonard J. Lobo, and Ke Cheng, June 17, 2021, Nature Nanotechnology.
DOI: 10.1038/s41565-021-00923-2
The research appears in Nature Nanotechnology and was supported by the National Institutes of Health and the American Heart Association. dr. Jason Lobo, pulmonologist at UNC-CH, co-authored the paper.
Authors: Zhenhua Li, Zhenzhen Wang, Phuong-Uyen C. Dinh, Dashuai Zhu, Kristen D. Popowski, Halle Lutz, Shiqi Hu, Ke Cheng, North Carolina State University; Leonard J. Lobo, University of North Carolina at Chapel Hill; Mark G. Lewis, Anthony Cook, Hanne Andersen, Jack Greenhouse, Laurent Pessaint, Bioqual, Inc.
Summary: Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has become a global pandemic and to date no specific antiviral treatments have been approved. The angiotensin-converting enzyme 2 (ACE2) plays a fundamental role in the pathogenesis of SARS-CoV-2 as it allows viral entry into host cells. Here we show that ACE2 nanodecoys derived from human spheroid lung cells (LSCs) can bind and neutralize SARS-CoV-2 and protect the host lung cells from infection. In mice, the nanodecoys were delivered via inhalation therapy and remained in the lungs for more than 72 hours after delivery. In addition, inhalation of nanodecoys accelerated the clearance of SARS-CoV-2 mimics from the lungs, with no observed toxicity. In cynomolgus macaques challenged with live SARS-CoV-2, four doses of nanodecoys released by inhalation promoted viral clearance and reduced lung damage. Our results suggest that LSC nanodecoys may serve as a potential therapeutic agent for the treatment of COVID-19.










