MIT’s New Carbon Nanotube-Based Sensor Can Detect COVID-19 or Other Emerging Pathogens
0 View
Share this Video
- Publish Date:
- 26 October, 2021
- Category:
- Covid
- Video License
- Standard License
- Imported From:
- Youtube
Tags
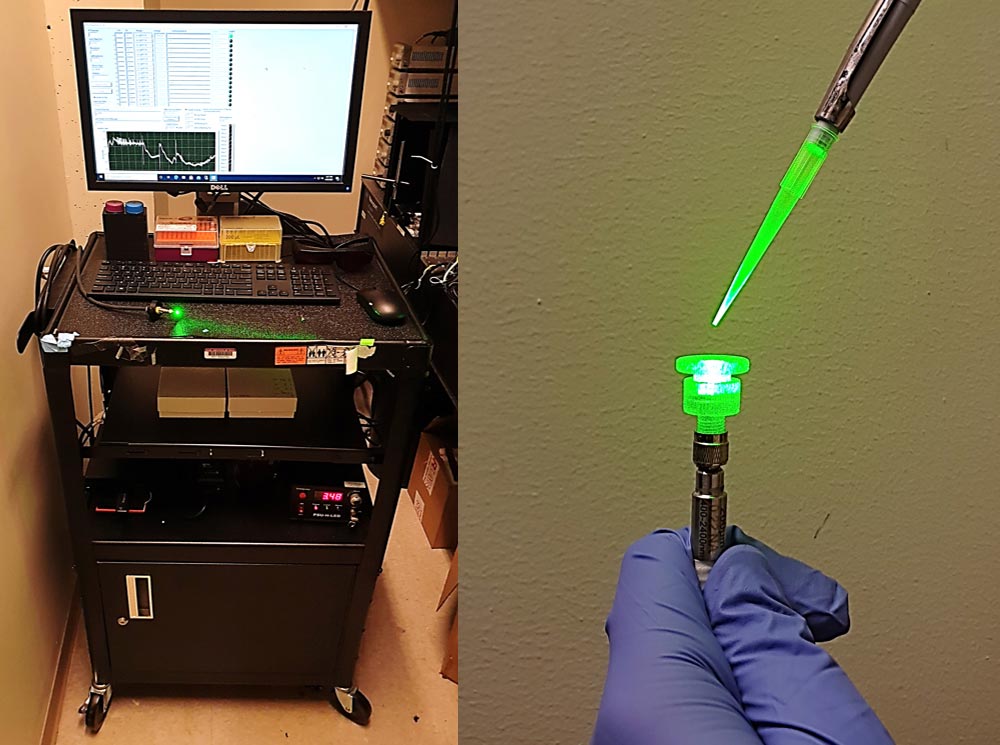
The researchers incorporated their sensor into a prototype with a fiberglass tip that can detect changes in fluorescence in the test sample. Credit: MIT
The technology could be developed as a rapid diagnosis for Covid-19 or other emerging pathogens.
Using specialized carbon nanotubes, MIT engineers have designed a new sensor that can detect SARS-CoV-2 without antibodies, yielding a result within minutes. Their new sensor is based on technology that can quickly generate rapid and accurate diagnostics not only for Covid-19 but also for future pandemics, the researchers say.
“A quick test means you can travel much earlier in a future pandemic. You can screen people getting off a plane and determine whether they should be quarantined or not. You could similarly screen people entering their workplace and so on,” said Michael Strano, the Carbon P. Dubbs Professor of Chemical Engineering at MIT and the study’s senior author. “We do not yet have technology that can develop and deploy such sensors quickly enough to prevent economic damage.”
The diagnosis is based on carbon nanotube sensor technology that Strano’s lab previously developed. Once the researchers started working on a Covid-19 sensor, it took them just 10 days to identify a modified carbon nanotube capable of selectively detecting the viral proteins they were looking for, and then targeting them. test and incorporate into a working prototype. This approach also eliminates the need for antibodies or other reagents that are time consuming to generate, purify and make widely available.
MIT postdoc Sooyeon Cho and graduate student Xiaojia Jin are the lead authors of the paper, which appears today (Oct. 26, 2021) in the journal Analytical Chemistry. Other authors include MIT graduate students Sungyun Yang and Jianqiao Cui, and postdoc Xun Gong.
Molecular Recognition
Several years ago, Strano’s lab developed a new approach to designing sensors for a variety of molecules. Their technique is based on carbon nanotubes – hollow, nanometer-thick cylinders made of carbon that naturally fluoresce when exposed to laser light. They have shown that by wrapping such tubes in various polymers, they can create sensors that respond to specific target molecules by chemically recognizing them.
Their approach, known as Corona Phase Molecular Recognition (CoPhMoRe), takes advantage of a phenomenon that occurs when certain types of polymers bind to a nanoparticle. Also called amphiphilic polymers, these molecules have hydrophobic regions that snap to the tubes as anchors and hydrophilic regions that form a series of loops extending away from the tubes.
Those loops form a layer called a corona that surrounds the nanotube. Depending on the arrangement of the loops, different types of target molecules can wedge into the spaces between the loops, and this target binding changes the intensity or peak wavelength of fluorescence produced by the carbon nanotube.
Earlier this year, Strano and InnoTech Precision Medicine, a Boston-based diagnostic developer, received a grant from the National Institutes of Health to create a CoPhMoRe sensor for SARS-CoV-2 proteins. Researchers in Strano’s lab had already developed strategies that would allow them to predict which amphiphilic polymers will interact best with a particular target molecule, so they were able to quickly generate a set of 11 strong candidates for SARS-CoV-2.
Within about 10 days of starting the project, the researchers had identified precise sensors for both the nucleocapsid and the spike protein of the SARS-CoV-2 virus. During that time, they were also able to incorporate the sensors into a prototype device with a fiber optic tip that can detect fluorescence changes from the biofluid sample in real time. This eliminates the need to send the sample to a lab, which is required for the gold standard PCR diagnostic test for Covid-19.
This device produces a result in about five minutes and can detect concentrations as low as 2.4 picograms of viral protein per milliliter of sample. In more recent experiments conducted after this paper was submitted, the researchers reached a detection limit lower than the rapid tests now commercially available.
The researchers also showed that the device could detect the SARS-CoV-2 nucleocapsid protein (but not the spike protein) when dissolved in saliva. Detecting viral proteins in saliva is usually difficult because saliva contains sticky carbohydrate and digestive enzyme molecules that interfere with protein detection. Therefore, most Covid-19 diagnostics require nasal swabs.
“This sensor exhibits the highest range of detection limit, response time, and saliva compatibility even without any antibody and receptor design,” says Cho. “It is a unique feature of this type of molecular recognition scheme that allows rapid design and testing, unfettered by the development time and supply chain requirements of a conventional antibody or enzymatic receptor.”
Quick response
The speed with which the researchers were able to develop a working prototype suggests that this approach could be useful for developing diagnostics more quickly during future pandemics, Strano says.
“We can go from someone handing us viral markers to a working fiber optic sensor in an extremely short time,” he says.
Sensors that rely on antibodies to detect viral proteins, which form the basis of many of the rapid Covid-19 tests now available, take much longer to develop because the process of designing the right protein antibody is so is time consuming.
The researchers have applied for a patent on the technology in hopes it could be marketed for use as a Covid-19 diagnosis. Strano also hopes to further develop the technology so that it can be rapidly deployed in future pandemics.
Reference: October 26, 2021, Analytical Chemistry.
The research was funded by a National Institutes of Health Rapid Acceleration of Diagnostics (RADx) grant.










