Lung Autopsies of COVID-19 Patients Reveal How Virus Spreads and Damages Tissue, Treatment Clues
0 View
Share this Video
- Publish Date:
- 25 November, 2021
- Category:
- Covid
- Video License
- Standard License
- Imported From:
- Youtube
Tags
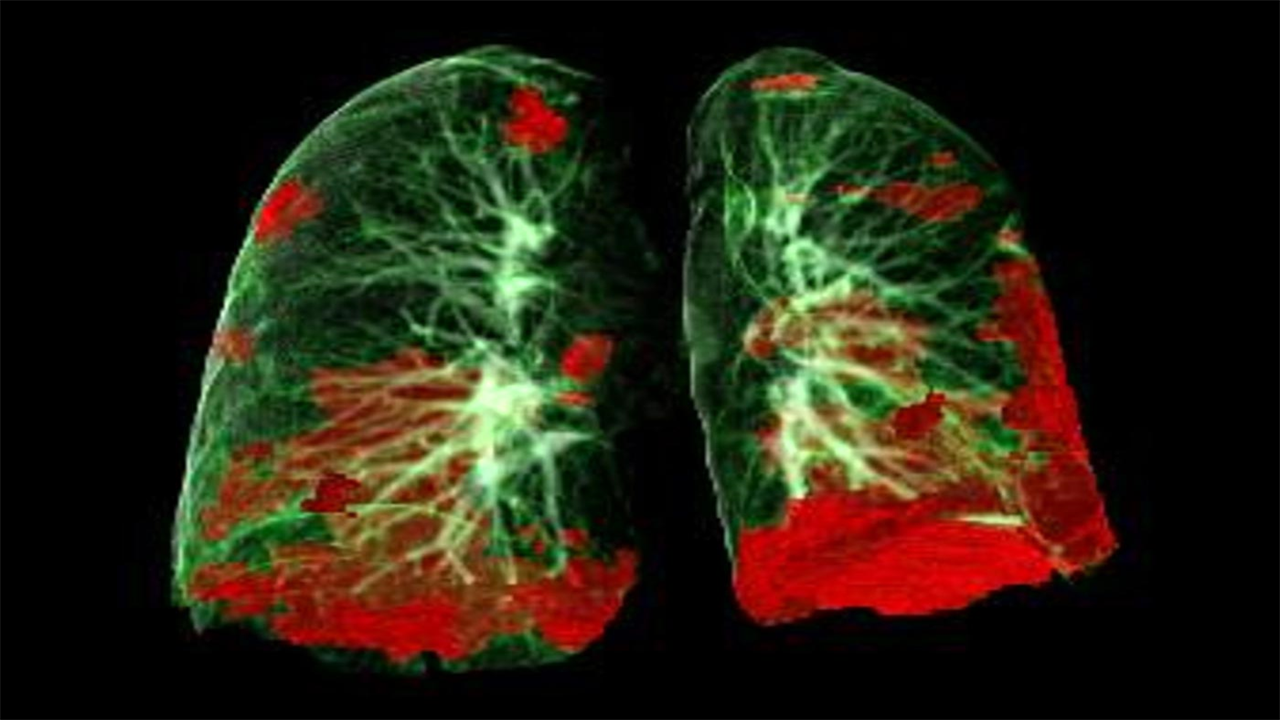
CT scan of the patient’s lungs with COVID-19 damage in red. Credit: Gerlig Widmann and team, Department of Radiology, Medical University of Innsbruck
SARS-CoV-2 prevents recovery, regeneration of lung tissue.
Lung autopsy and plasma samples from people who died from COVID-19 have provided a clearer picture of how the SARS-CoV-2 virus spreads and damages lung tissue. Scientists at the National Institutes of Health and their collaborators say the information, published in Science Translational Medicine, could help predict severe and long-term cases of COVID-19, particularly in high-risk people, and develop effective treatments. to inform.
Although the study was small — lung samples from 18 cases and plasma samples from six of those cases — the scientists say their data revealed trends that could help develop new COVID-19 therapies and refine their use. of existing therapies at different stages of disease progression. The findings include details of how SARS-CoV-2, the virus that causes COVID-19, spreads in the lungs, manipulates the immune system, causes widespread thrombosis that does not resolve and targets signaling pathways that cause lung failure, fibrosis and damage. tissue repair. The researchers say the data is particularly relevant to care for COVID-19 patients who are elderly, obese or have diabetes — all considered high-risk populations for severe cases. Study samples were from patients who had at least one high-risk condition.
Colorized scanning electron micrograph of a cell infected with a variant strain of SARS-CoV-2 virus particles (blue), isolated from a patient sample. Image taken at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
The study included patients who died between March and July 2020, with time of death ranging from three to 47 days after symptoms began. This varied time frame allowed the scientists to compare short-, medium- and long-term cases. Each case showed findings consistent with diffuse alveolar damage, which prevents proper oxygenation to the blood and eventually thickens and stiffens the lungs.
They also found that SARS-CoV-2 directly infected basal epithelial cells in the lungs, hampering their essential function of repairing damaged airways and lungs and generating healthy tissue. The process is different from the way flu viruses attack cells in the lungs. This provides scientists with additional information they can use when evaluating or developing antiviral therapies.
Researchers from the NIH’s National Institute of Allergy and Infectious Diseases led the project in collaboration with the National Institute of Biomedical Imaging and Bioengineering and the US Food and Drug Administration. Other contributors included the Institute for Systems Biology in Seattle; University of Illinois, Champaign; Saint John’s Cancer Institute in Santa Monica, Calif.; the USC Keck School of Medicine in Los Angeles; University of Washington Harborview Medical Center, Seattle; University of Vermont Medical Center, Burlington; and Memorial Sloan Kettering Cancer Center in New York City.
Reference: “Lung epithelial and endothelial damage, loss of tissue repair, inhibition of fibrinolysis and cellular aging in fatal COVID-19” by Felice D’Agnilo, Kathie-Anne Walters, Yongli Xiao, Zong-Mei Sheng, Kelsey Scherler, Jaekeun Park, Sebastian Gygli, Luz Angela Rosas, Kaitlyn Sadtler, Heather Kalish, Charles A. Blatti, Ruoqing Zhu, Lisa Gatzke, Colleen Bushell, Matthew J. Memoli, Steven J. O’Day, Trevan D. Fischer, Terese C. Hammond , Raymond C. Lee, J. Christian Cash, Matthew E. Powers, Grant E. O’Keefe, Kelly J. Butnor, Amy V. Rapkiewicz, William D. Travis, Scott P. Layne, John C. Kash and Jeffery K Taubenberger, October 14, 2021, Science Translational Medicine.
DOI: 10.1126/scitranslmed.abj7790
Jeffrey Taubenberger, MD, Ph.D., chief of the Division of Viral Pathogenesis and Evolution in NIAID’s Laboratory of Infectious Diseases, is available to discuss this study.










