Early Antiviral Response in the Nose May Determine Mild / Severe Course of COVID-19
0 View
Share this Video
- Publish Date:
- 24 July, 2021
- Category:
- Covid
- Video License
- Standard License
- Imported From:
- Youtube
Tags
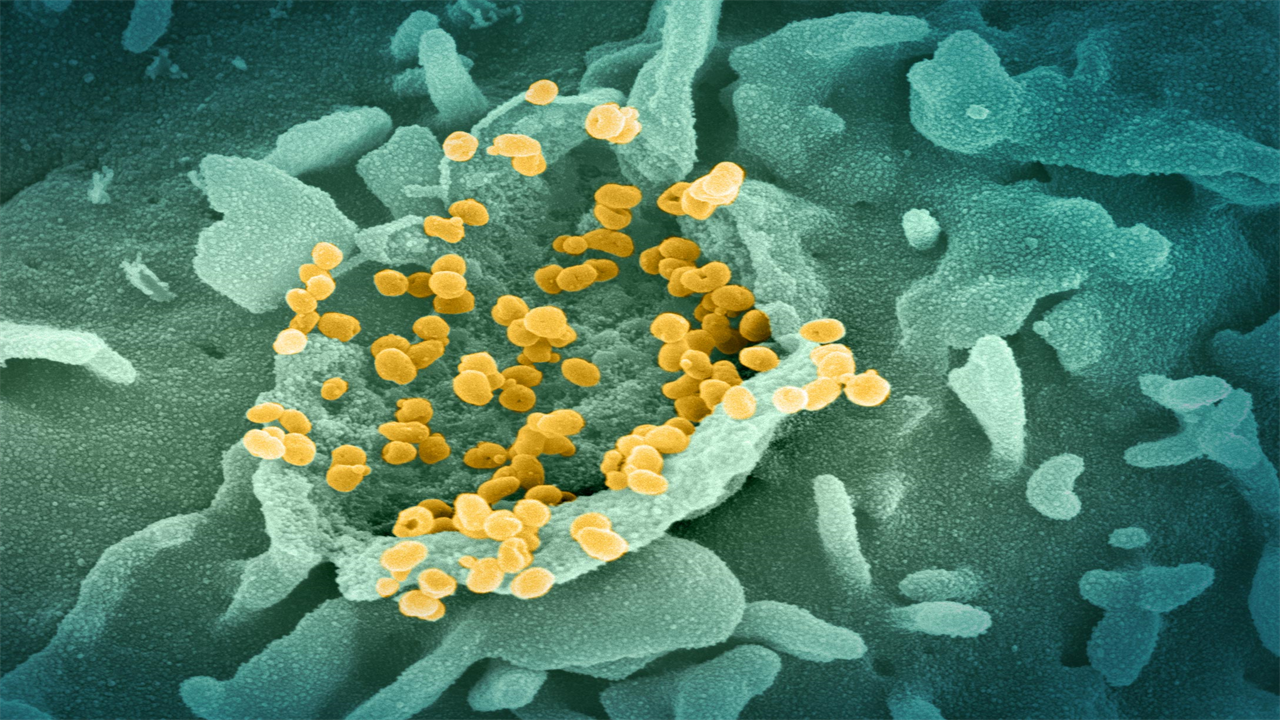
This scanning electron microscope image shows SARS-CoV-2 (spherical gold particles) emerging from the surface of a cell grown in the lab. Image captured and colored at Rocky Mountain Laboratories in Hamilton, Montana. Credit: NIAID
Cells taken from patients at time of diagnosis who later developed severe COVID-19 show muted antiviral response, study finds.
Researchers studied cells collected by nasal swabs at the time of diagnosis for both mild and severe COVID-19 patients. Cells taken from patients who developed severe disease had a muted antiviral response compared to those who developed mild disease. This suggests it may be possible to develop early interventions that prevent severe COVID-19 from developing. The team also identified infected host cells and pathways associated with protection against infection that may enable novel therapeutic strategies for COVID-19 and other respiratory viral infections.
Over the past 18 months, researchers have learned a lot about COVID-19 and its viral cause, SARS-CoV-2. They know how the virus enters the body, enters through the nose and mouth, and the infection begins in the mucous layers of the nasal passage. They know that infections that stay in the upper respiratory tract are likely to be mild or asymptomatic, while infections that travel through the airways to the lungs are much more serious and can lead to fatal illness. And they have identified common risk factors for serious diseases, such as age, gender and obesity. But there are still many unanswered questions, such as when and where the course of severe COVID-19 is determined. Does the road to serious illness begin only after the body has failed to get the mild illness under control, or can it begin much earlier?
Researchers from the Ragon Institute of MGH, MIT and Harvard; the Broad Institute at MIT and Harvard; Boston Children’s Hospital (BCH); MIT; and the University of Mississippi Medical Center (UMMC) wondered whether this path to serious illness could begin much earlier than expected — perhaps even within the initial response created when the virus enters the nose.
To test this, they studied cells taken from nasal swabs from patients at the time of their initial COVID-19 diagnosis, comparing patients who developed mild COVID-19 with those who progressed to more severe disease and eventually needed respiratory support. . Their results showed that patients who developed severe COVID-19 showed a much more muted antiviral response in the cells collected from those early smears, compared to patients with a mild course of disease. The article appears in the journal Cell.
“We wanted to understand whether there were pronounced differences in samples taken early in the disease course that were associated with different severity of COVID-19 as the disease progressed,” said co-senior author José Ordovás-Montañés, an associate member of the Klarman Cell Observatory at Broad and assistant professor at BCH and Harvard Medical School. “Our findings suggest that the course of severe COVID-19 may be determined by the body’s intrinsic antiviral response to the initial infection, opening new avenues for early interventions that can prevent serious disease.”
To understand the early response to infection, Sarah Glover of UMMC’s Division of Digestive Diseases and her lab collected nasal swabs from 58 people. Thirty-five swabs were taken from COVID-19 patients at the time of diagnosis, representing a variety of disease states, from mild to severe. Seventeen swabs were collected from healthy volunteers and six from patients with respiratory failure due to other causes. The team isolated individual cells from each sample and sequenced them, looking for RNA that would indicate what kind of proteins the cells were making — a proxy for understanding what a particular cell is doing at the time of collection.
Cells use RNA as instructions to make proteins – tools, machines and building blocks used in and by the cell to perform various functions and respond to its environment. By studying the collection of RNA in a cell – the transcriptome – researchers understand how a cell reacts at that specific moment to changes in the environment, such as a viral infection. Researchers can even use the transcriptome to see if individual cells are infected with an RNA virus such as SARS-CoV-2.
Alex Shalek, co-senior author of the study, a member of the Ragon Institute of MGH, MIT and Harvard, and an institute member at Broad, specializes in studying the transcriptomes of individual cells. His lab has helped develop innovative approaches to sequence thousands of individual cells from low-input clinical samples, such as the nasal swab from COVID-19 patients, and uses the resulting data to create high-resolution pictures of the orchestrated response. of the body for infection at the sample site.
“Our single-cell sequencing approaches allow us to comprehensively study the body’s response to disease at a specific point in time,” said Shalek, who is also an associate professor at MIT in the Institute for Medical Engineering & Science, the Department of Chemistry, and the Koch Institute for Integrative Cancer Research. “This gives us the opportunity to systematically examine characteristics that distinguish one disease course from another, as well as cells that are infected from those that are not. We can then use this information to develop more effective preventions and treatments for COVID-19.” and other viral infections.”
Ordovás-Montañés’ lab studies inflammatory responses and their memory, specializing in those found in epithelial cells — the top layer of cells, like those lining your nasal passages and collected by nasal swabs. In collaboration with the Shalek lab and that of Bruce Horwitz, a senior associate physician in the BCH Division of Emergency Medicine, the researchers questioned how both epithelial and immune cells responded to early COVID-19 infection from the single-cell transcriptome data.
First, the team found that the antiviral response, driven by a family of proteins called interferons, was much more muted in patients who developed severe COVID-19. Second, patients with severe COVID-19 had higher amounts of highly inflammatory macrophages, immune cells that contribute to high amounts of inflammation, often found in severe or fatal COVID-19.
Since these samples were taken well before COVID-19 had reached its maximum disease state in the patients, both findings indicate that the course of COVID-19 can be determined by the initial or very early response of the nasal epithelium and immune cells to the virus. The lack of a strong initial antiviral response allows the virus to spread more quickly, increasing its chances of moving from the upper to lower respiratory tract, while the recruitment of inflammatory immune cells could fuel the dangerous inflammation in serious diseases.
Finally, the team also identified infected host cells and pathways associated with protection against infection — cells and responses unique to patients who developed mild disease. These findings may enable researchers to discover new therapeutic strategies for COVID-19 and other respiratory viral infections.
If, as the team’s evidence suggests, the early stages of infection can determine the disease, it will open a path for scientists to develop early interventions that can help prevent severe COVID-19 from developing. The team’s work even identified potential markers of severe disease, genes expressed in mild COVID-19 but not severe COVID-19.
“Almost all of our severe COVID-19 samples lacked the expression of several genes that we would normally expect in an antiviral response,” said Carly Ziegler, a graduate student in the Health Science and Technology program at MIT and Harvard and one of the fellow students of the study. -first authors. “If further studies support our findings, we could use the same nasal swabs we use to diagnose COVID-19 to identify potentially serious cases before serious disease develops, creating an opportunity for effective early intervention.”
Reference: “Decreased local intrinsic immunity to SARS-CoV-2 infection in severe COVID-19” by Carly GK Ziegler, Vincent N. Miao, Anna H. Owings, Andrew W. Navia, Ying Tang, Joshua D. Bromley, Peter Lotfy , Meredith Sloan, Hannah Laird, Haley B. Williams, Micayla George, Riley S. Drake, Taylor Christian, Adam Parker, Campbell B. Sindel, Molly W. Burger, Yilianys Pride, Mohammad Hasan, George E. Abraham III, Michal Senitko, Tanya O. Robinson, Alex K. Shalek and Sarah C. Glover, July 22, 2021, Cell.
DOI: 10.116/j.cell.2021.07.023
This study was supported by the Chan Zuckerberg Initiative, the Richard and Susan Smith Family Foundation, the AGA Research Foundation, the New York Stem Cell Foundation, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of General Medical Sciences, the National Institute on Aging, the Leona M. and Harry B. Helmsley Charitable Trust, the Crohn’s and Colitis Foundation, the Ragon Institute of MGH, MIT and Harvard, and other sources.










