Did the CDC’s COVID-19 Vaccine Strategy Work? Comparing 17.5 Million Options
0 View
Share this Video
- Publish Date:
- 17 November, 2021
- Category:
- Covid
- Video License
- Standard License
- Imported From:
- Youtube
Tags
The first doses of Pfizer’s Covid-19 vaccine will be delivered to healthcare workers at Iowa State University on Friday, December 18, 2020 at the Thielen Student Health Center. Credit: Christopher Gannon/Iowa State University
A year ago, amid surging COVID-19 cases and a limited supply of newly developed vaccines, the U.S. Centers for Disease Control and Prevention faced a big question: Who should be first in line to get a to get a vaccine? Students living in dorms or people with chronic kidney disease? Grandmas or teachers? Along with goals to reduce overall infections and deaths, the CDC wanted to prevent hospitals from becoming overwhelmed and ensure equitable access to COVID-19 vaccines.
Researchers from Iowa State University were part of a team that evaluated 17.5 million potential strategies that the CDC could have recommended last winter to state, territorial, tribal and local governments for the rollout of COVID-19 vaccines. In a newly published paper, the researchers generally validate the CDC’s ultimate recommendation, while the mathematical model the team developed also highlights some minor improvements. The work could help design future vaccination strategies in the US and abroad.
The CDC has recommended four staggered priority groups for COVID-19 vaccines:
Phase 1a included healthcare staff and residents of long-term care facilities. Phase 1b included essential frontline workers who do not work in health care (e.g., police officers, firefighters, child caregivers) and people aged 75 years and older. Phase 1c included other essential workers (e.g. bus drivers, bank clerks), 16-64 year olds at increased risk of severe COVID-19 disease and 65-74 year olds. Phase 2 included 16-64 year olds with no high-risk conditions or co-morbidities.
“The CDC strategy did very well when we compared it to all the other possible strategies, especially in preventing deaths in different age groups,” said Claus Kadelka, an assistant professor of mathematics and the corresponding author of the paper published in PLOS ONE. . “Our research shows that the CDC’s prioritization of essential frontline workers, people in older age groups, and those with underlying health conditions was a highly effective strategy for reducing COVID-19 mortality while keeping the overall number of cases at bay. .”
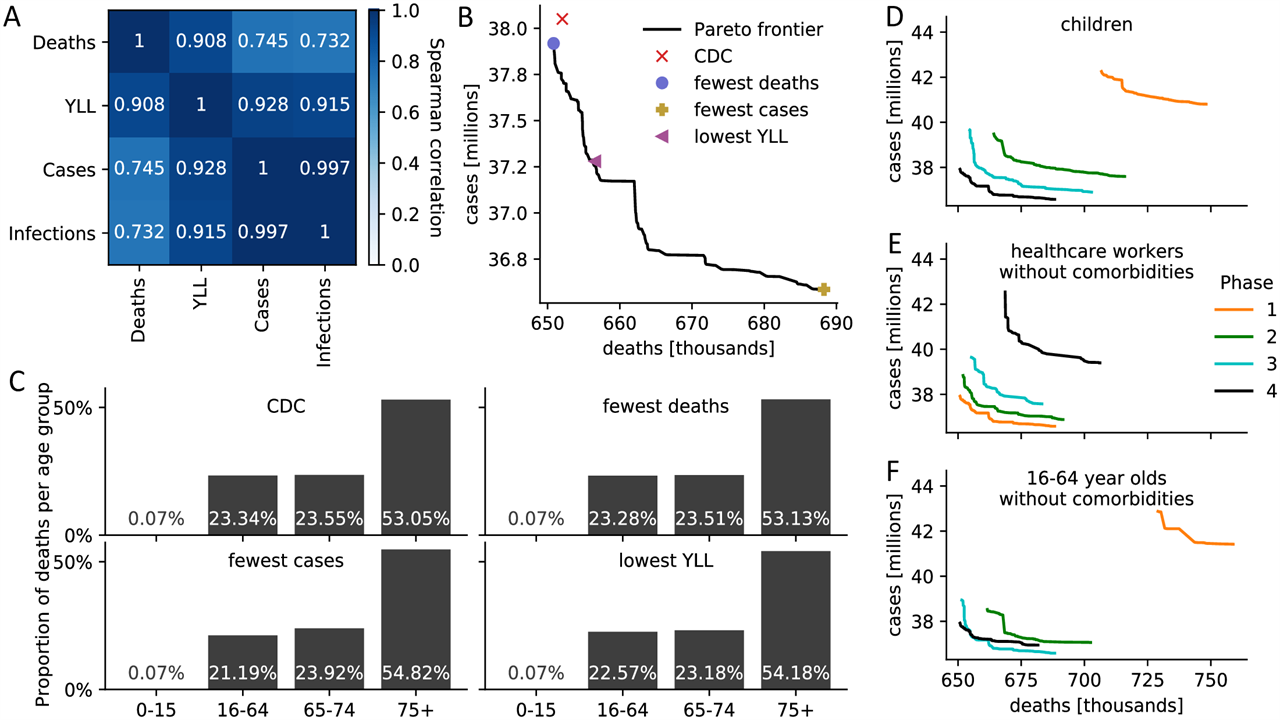
(A) Spearman correlation between four measures of disease burden based on a full comparison of all 17.5 million meaningful four-phase vaccine delivery strategies. (B) Pareto boundary of all optimal strategies based on a global search of all 17.5 million meaningful vaccine allocation strategies. For strategies on the Pareto frontier, there is no other strategy that performs better in one target (minimizing the number of deaths or cases) while not performing worse in the other target. The number of deaths and cases due to four specific assignments is highlighted. (C) For the four strategies highlighted in (B), the distribution of all resulting deaths across the four age groups is presented as a measure of equity. (DF) Pareto limits of all optimal strategies are shown when restricting (D) children, (E) health professionals with no comorbidities, (F) 16-64 year-olds with no comorbidities and without an essential occupation to a certain priority stage. S8 Fig contains Pareto boundaries for all subpopulations. Credit: Islam et al., 2021, PLOS ONE, CC-BY 4.0
To evaluate the CDC’s recommendations, Kadelka and the research team built a mathematical model that spanned the agency’s four staggered phases of vaccine rollout and 17 subpopulations based on factors such as age, living conditions and occupation. Individuals fell into one of 20 categories, such as “susceptible to the virus,” “fully vaccinated,” “currently infected,” “infected but without COVID-19 symptoms,” and “recovered.” The researchers also took into account several key features of the COVID-19 pandemic, such as vaccine hesitancy, social distancing levels based on current caseloads in the US, and different infection rates for different virus variants.
“We ran the model 17.5 million times on the ISU supercomputer and for each run we recorded and compared different outcome metrics: the predicted number of deaths, the predicted number of cases, and so on,” Kadelka said.
Vaccinating children in a phase other than the last phase of the vaccine roll-out always led to a non-optimal result in the model. The researchers said the CDC’s recommendations could have been optimal if more individuals with known COVID-19 risk factors had been prioritized over those in their cohort without health risks. However, the gains would have been small (i.e. less than 1% fewer deaths and total life years lost, and 4% fewer cases and infections), and Kadelka said the model doesn’t account for potential logistical challenges.
“We don’t know enough about the situation in nursing homes to know how easy it would be to distinguish which residents have greater risk factors that would put them at the forefront of the vaccination line. That’s something you can do in a mathematical model, but in practice it can be difficult,” added Kadelka.
Kadelka said part of what makes the model unique is that it takes into account the degree to which a vaccine prevents someone from becoming infected, developing symptoms and passing the virus on to others, all of which can change or even change over time. may vary depending on the specific vaccine. The researchers show that the ideal vaccination strategy is sensitive to these largely unknown parameters.
Md. Rafiul Islam, a postdoc in Kadelka’s group and the paper’s lead author, said the mathematical model could help design current and future vaccination strategies.
“Our model is useful to identify an optimal vaccine allocation strategy and can be easily extended to answer questions related to booster allocation in the face of declining immunity and increasing virus variability,” Islam said.
Kadelka added: “If the (SARS-CoV-2) virus mutates enough to render current vaccines ineffective or if we have a new pandemic, whether that is in 100 years or two years, we should be able to accurately predict what the outcome will be when it is decided who will be vaccinated first.”
Developing a vaccine strategy is complicated and there will always be trade-offs between opposing goals, such as minimizing mortality or incidence. But Kadelka believes mathematical models like the one he and his colleagues have created can ensure that life-saving vaccines can have the greatest impact.
Reference: “Assessment of the United States COVID-19 Vaccine Allocation Strategy” Nov 17, 2021, PLoS ONE.
DOI: 10.1371/journal.pone.0259700










