Did the CDC’s COVID-19 Vaccine Prioritization Strategy Work?
0 View
Share this Video
- Publish Date:
- 21 November, 2021
- Category:
- Covid
- Video License
- Standard License
- Imported From:
- Youtube
Tags
The CDC’s vaccine prioritization strategy performed well compared to other approaches, although there was some room for improvement.
The four-pronged vaccine prioritization strategy implemented by the U.S. Centers for Disease Control and Prevention (CDC) performed well through many measures, but could be improved, compared to all possible approaches to COVID-19 vaccine rollout . The results are published this week in a new study in the open-access journal PLOS ONE by Md Rafiul Islam and Claus Kadelka of Iowa State University, USA, and colleagues.
Anticipating an initial shortage of vaccines for COVID-19, the U.S. Centers for Disease Control (CDC) have developed priority vaccine allocations for specific demographic groups in the population. This prioritization strategy, and its impact on subsequent disease, has been studied in many ways, but generally only compared to a small number of other vaccine deployment strategies at the same time.
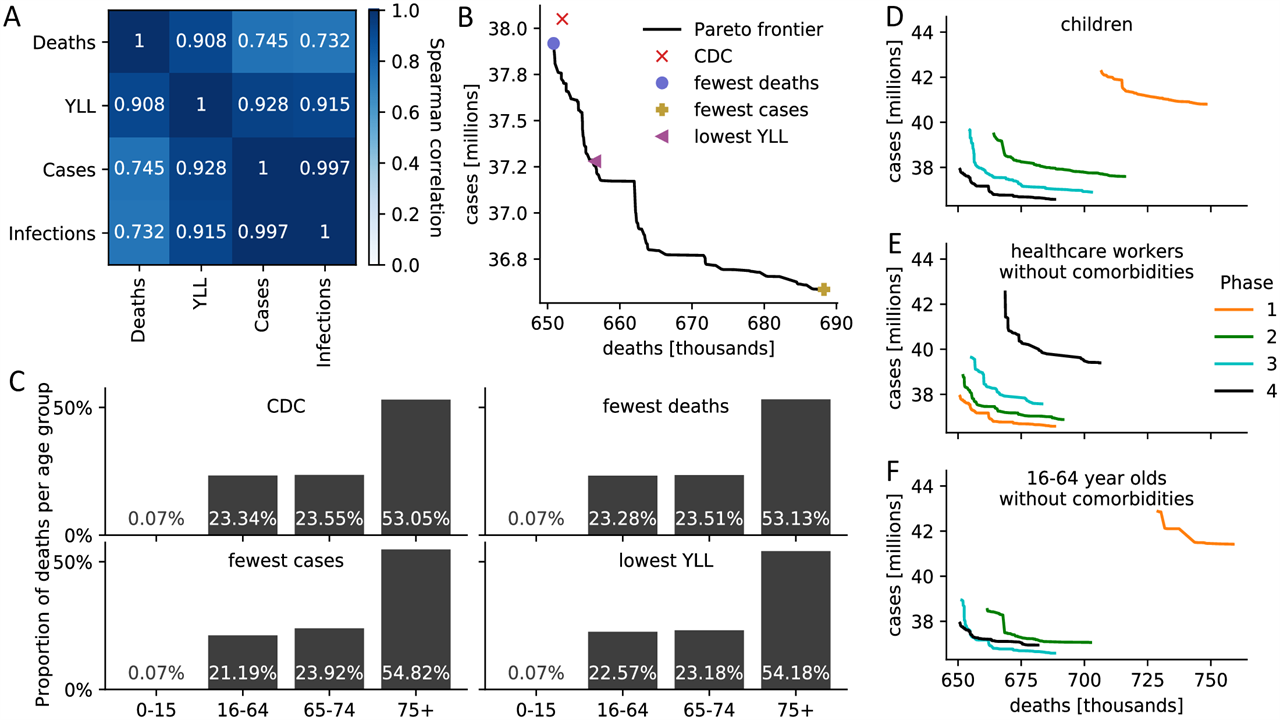
(A) Spearman correlation between four measures of disease burden based on a full comparison of all 17.5 million meaningful four-phase vaccine delivery strategies. (B) Pareto boundary of all optimal strategies based on a global search of all 17.5 million meaningful vaccine allocation strategies. For strategies on the Pareto frontier, there is no other strategy that performs better in one target (minimizing deaths or cases) while not performing worse in the other target. The number of deaths and cases due to four specific assignments is highlighted. (C) For the four strategies highlighted in (B), the distribution of all resulting deaths across the four age groups is presented as a measure of equity. (DF) Pareto limits of all optimal strategies are shown when restricting (D) children, (E) health professionals with no comorbidities, (F) 16-64 year-olds with no comorbidities and without an essential occupation to a certain priority stage. S8 Fig contains Pareto boundaries for all subpopulations. Credit: Islam et al., 2021, PLOS ONE, CC-BY 4.0
In the new study, Kadelka and colleagues developed a disease model that divided the US population into 17 subpopulations based on the characteristics listed in the CDC vaccine recommendation — age, co-morbidity status, work type, and living situation. There are a total of approximately 17.2 billion ways to assign vaccines to these 17 subpopulations in up to four stages. The researchers found that only 17.5 million can be optimal. They compared these 17.5 million allocation strategies and analyzed the resulting effect on COVID-19 cases, mortality and lost life years (YLL), using established assumptions about the incubation and spread of COVID-19, vaccine hesitancy and vaccine effectiveness rates. .
According to the analysis, the CDC allocation strategy performed well across all vaccination targets, but never scored the highest of all possible strategies. Compared to the respective optimal methods, the CDC approach resulted in an estimated 0.19% more deaths, 4.0% more cases, 4.07% more infections and 0.97% higher YLL. Note that there are trade-offs between the vaccination goals, so that no single strategy performs best in the objectives: for example, low death rates come at the expense of higher numbers of cases. The CDC’s decision not to prioritize vaccination of those under 16 was optimal, as was the priority of health professionals and other essential workers. However, theoretical strategies that prioritized vaccination of individuals with co-morbidities in all age groups were considered to improve outcomes. The authors believe that this optimization approach can be used to inform the design of future strategies for vaccine allocation around the world.
The authors add, “We have developed a model that allows for an accurate evaluation of COVID-19 vaccine prioritization in the United States. The model further shows how the choice of an optimal vaccine strategy depends on parameters such as hesitation or how a specific vaccine functions.”
To learn more about this study, read Did the CDC’s COVID-19 Vaccine Strategy Work? Comparison of 17.5 million options.
Reference: “Evaluation of the COVID-19 Vaccine Allocation Strategy in the United States” by Md Rafiul Islam, Tamer Oraby, Audrey McCombs, Mohammad Mihrab Chowdhury, Mohammad Al-Mamun, Michael G. Tyshenko and Claus Kadelka, 17 Nov 2021, PLoS ONE.
DOI: 10.1371/journal.pone.0259700










