Cells Damaged by Chronic Lung Disease Can Result in Severe COVID
0 View
Share this Video
- Publish Date:
- 14 July, 2021
- Category:
- Covid
- Video License
- Standard License
- Imported From:
- Youtube
Tags
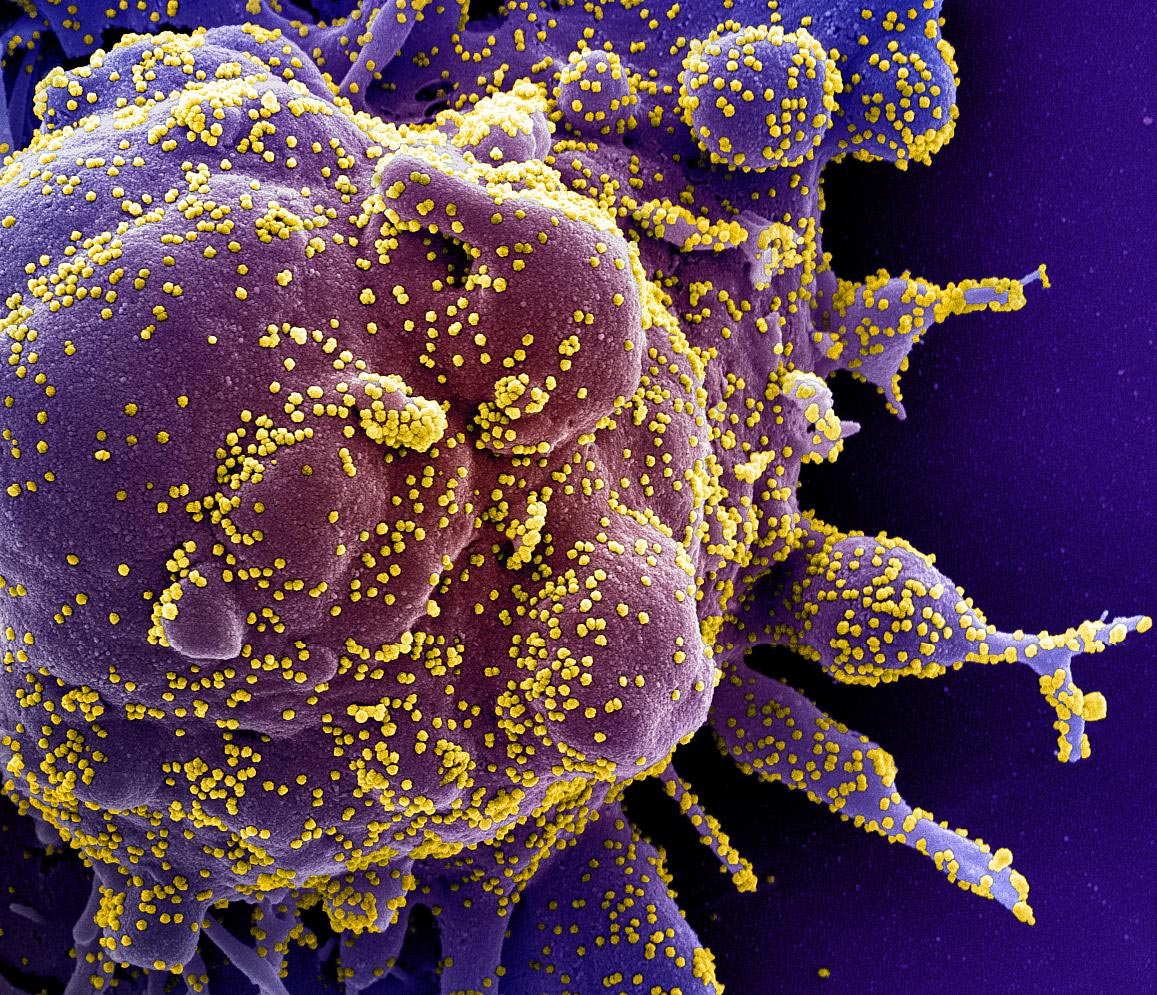
Stained scanning electron micrograph of a cell (purple) heavily infected with SARS-COV-2 virus particles (yellow), isolated from a patient sample. Image taken at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
Results from a TGen-led international study suggest that SARS-CoV-2 benefits from genetic alterations in patients with pre-existing lung diseases.
The results of a study by an international scientific team led by the Translational Genomics Research Institute (TGen), an affiliate of the City of Hope, suggest that—much like pouring water onto a well before pumping it—the airway cells of patients with chronic pneumonia Diseases are ‘prepared’ for infection by the COVID-19 virus, resulting in more severe symptoms, worse outcomes and a greater chance of death.
The study – published today in Nature Communications – describes the genetic changes caused by chronic lung disease in the molecular makeup of a variety of cells, including the epithelial cells that line the lungs and airways. The study details how those changes could help SARS-CoV-2, the virus that causes COVID-19, get into the body, replicate and trigger an uncontrollable immune response that fills the lungs with fluid and often results in patients requiring ventilators. and require long hospital stays.
The team used single-cell RNA sequencing technology to describe the genetic code of 611,398 cells from various databases, representing both those with healthy (control) lungs and those with chronic lung disease. Sequencing and analysis allowed researchers to identify molecular features that may be the cause of worse COVID-19 outcomes.
“Our results suggest that patients with chronic lung disease are molecularly primed to be more susceptible to infection by SARS-CoV-2,” said Nicholas Banovich, Ph.D., an associate professor in TGen’s Integrated Cancer Genomics Division, and one of the senior authors of the study. dr. Banovich is a leading participant in the Human Cell Atlas Lung Biological Network, whose dozens of members, representing more than 80 institutions worldwide, also contributed to this research.
In addition, older age, male gender, smoking, and co-morbidities such as high blood pressure, obesity, and diabetes are all COVID-19 risk factors that are exacerbated by chronic lung diseases, such as Chronic Obstructive Pulmonary Disease (COPD), Interstitial Lung Disease (ILD), and in particular idiopathic pulmonary fibrosis (IPF), a progressive scarring and stiffening of the lung tissue.
“It was recognized early in the pandemic that patients with chronic lung disease were at particularly high risk for severe COVID-19, and our goal was to understand the cellular and molecular changes responsible for this,” said Jonathan Kropski, MD, Associate Professor of Medicine and Cell and Developmental Biology at Vanderbilt University Medical Center, and a co-senior author of the study.
Changes in lung cells and immune cells
Researchers specifically looked for changes in AT2 cells, an important lung epithelial cell type, focusing on cellular pathways and expression levels of genes associated with COVID-19. They determined a “viral entry score,” a composite of all genes associated with SARS-CoV-2, and found higher scores in cells from patients with chronic lung disease.
They also examined changes in immune cells and found dysregulated gene expression associated with hyperinflammation and with sustained cytokine production, two hallmark symptoms of severe SARS-CoV-2 infection. So-called cytokine storms in COVID-19 patients unleash a cascade of immune cells that flood the lungs, causing severe organ damage.
“The genetic changes in immune cells, especially in specialized white blood cells known as T cells, may decrease the patient’s immune response to viral infection and lead to a higher risk of serious disease and poor outcomes in patients with chronic lung disease. Linh Bui said. , Ph.D., a postdoctoral researcher in Dr. Banovich, and one of the study’s lead authors.
“Our data suggest that the immune microenvironment at both the molecular and cellular levels in lungs damaged by chronic disease may promote severe COVID-19,” said Dr. Shower.
Reference: July 14, 2021, Nature Communications.
DOI: 10.1038/s41467-021-24467-0
Significant contributions to this study were made by: Vanderbilt University Medical Center, Yale School of Medicine, Harvard Medical School, Baylor College of Medicine, and the Department of Veterans Affairs Medical Center. Plus several institutes in the UK including: London’s Imperial College, Royal Brompton and Harefield National Health System Foundation Trust, Edinburgh University Medical School and the Royal Infirmary of Edinburgh.
Major funding for this study – chronic lung diseases are associated with gene expression programs that promote SARS-CoV-2 access and severity – was provided by the National Institutes of Health, the Department of Defense, the Department of Veterans Affairs and the Doris Duke Charitable Foundation .










