Autoimmune Antibodies Could Predict COVID-19 Severity
0 View
Share this Video
- Publish Date:
- 9 September, 2021
- Category:
- Covid
- Video License
- Standard License
- Imported From:
- Youtube
Tags
The presence of special immune defense molecules called autoimmune antibodies is strongly linked to how badly people do when they are hospitalized with COVID-19, a new study shows.
Led by researchers at the NYU Grossman School of Medicine, the study detected the autoimmune antibodies in the blood of more than a third of men and women upon hospitalization and confirmed the disease.
One of the new research findings is that a subset of these autoimmune antibodies that bind to DNA or to a certain type of fat molecule, a lipid called phosphatidylserine, was more likely to be twice as abundant at the start of a coronavirus infection in those whose condition deteriorated rapidly. than in those whose health did not deteriorate. Patients with these elevated levels of autoimmune antibodies were five to seven times more likely to develop serious disease than those whose antibody levels were stable.
People hospitalized with life-threatening cases of COVID-19, researchers said, required intensive care and a mechanical ventilator to help them breathe, while those with lower levels of these autoantibodies tended to breathe on their own and largely recovered.
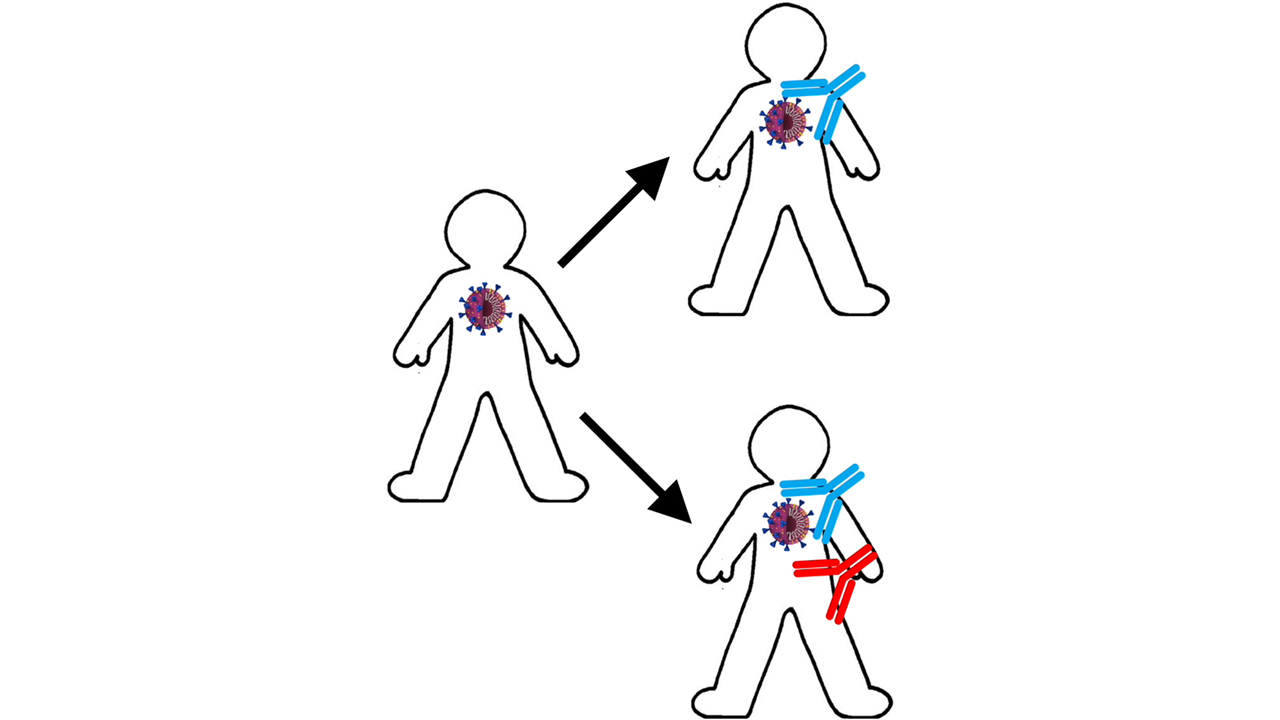
The team’s latest work, published online today (Sept. 9, 2021) in the journal Life Science Alliance, is based on the nature of antibodies, they explain, immune proteins that target invading bacteria and viruses. In contrast, autoimmune antibodies instead attack an infected person’s own cells and molecules. This includes lipids and genetic material, or DNA, which are known to enter the bloodstream when cells are killed by a disease, such as COVID-19.
“Our study results show that initial blood levels of anti-DNA or anti-phosphatidylserine antibodies were directly related to disease severity in people with COVID-19,” said co-lead researcher Claudia Gomes, PhD, a postdoctoral researcher. the NYU Langone Health.
“While further testing is needed, our findings suggest that testing for the presence of anti-DNA and anti-phosphatidylserine antibodies could help identify those hospitalized COVID-19 patients who are most are at risk of needing intensive care and need treatment. monitored more closely,” said Marisol Zuniga, MS, also a co-principal investigator of the study at NYU Langone.
For the new study, researchers examined the medical records and blood tests of 115 white, black, Asian and Hispanic men and women hospitalized for COVID-19 at NYU Langone hospitals between April and June 2020. About equal numbers had a serious illness from which she either survived or died, or did not require intensive care and recovered quickly. Test results for more than 100 measurements, such as blood oxygen levels, liver enzymes and kidney function, were compared with levels of autoimmune antibodies.
The researchers designed the analysis to find out whether common autoimmune antibodies were present in COVID-19, as other studies of other infectious diseases had suggested, and whether or not variations in blood levels were related to how sick people became.
Thirty-six percent of the study participants were found to have autoimmune antibodies when they were hospitalized. Levels of anti-DNA and anti-phosphatidylserine antibodies were then strongly linked to disease severity. Specifically, 86 and 93 percent of patients with high levels of anti-DNA and anti-phosphatidylserine antibodies, respectively, experienced severe COVID-19. Levels of anti-DNA antibodies have also been linked to increased blood clotting (thrombosis) and cell death (lysis), especially in muscle tissue. Researchers say both thrombosis, which can lead to life-threatening blood clots, and damage to muscle tissue, especially in the heart, have been observed in the most severe cases of COVID-19.
“Our general observations suggest that in severe cases of COVID-19, autoimmune antibody production plays a key role in blood clotting and cell death,” said senior researcher Ana Rodriguez, PhD, a professor in the Department of Microbiology at NYU Langone. “Our study adds evidence to the underlying premise of the disease that the misguided immune system’s response does more damage than the actual viral infection itself.”
Rodriguez warns that further experiments will be needed to determine whether autoimmune antibodies are indeed the “cause or effect” of the blood clotting and cell lysis observed in her team’s study.
If determined to be causal for cell damage, new COVID-19 treatments may include antibody injections from healthy donors to dilute the presence of autoimmune antibodies. Other experimental therapies under consideration include biodegradable antigens that attach to and neutralize autoimmune antibodies, but do not lead to a lasting self-antibody immune response.
Reference: “Autoimmune anti-DNA antibodies in COVID-19 patients are associated with thrombosis and cell lysis” September 9, 2021, Life Science Alliance.
DOI: 10.26508 / lsa.202101180
Student grants were provided by NYU Langone.
In addition to Gomes, Zuniga, and Rodriguez, Kun Qian, Kelly Crotty, Laurance Hsu Lin, Kimon Argyropoulos, Huilin Li, Paolo Cotzia, Robert Clancy, Peter Izmirly, Jill Buyon, and David C. Lee are other researchers from NYU Langone involved in this study. to be. . Other research researchers include Nubia Catalina-Tovar and Maria Fernanda Yasnot-Acosta at the University of Cordoba in Colombia.










